Introduction
Patient and family collaborators offer unique insights and real-world perspectives that significantly enhance the relevance and impact of Quality Improvement (QI) projects. Involving stakeholders in all phases of a QI project has several benefits, including enhancing the project’s design/feasibility, ensuring that outcome metrics matter to patients/families, transforming data into actionable insights, increasing the cultural relevance of patient- and family-facing processes, and addressing health disparities (Batalden, 2018; O’Brien et al., 2021). Additionally, centering efforts around the patient and family voice promotes transparency and accountability in the process (Harrison et al., 2019).
Engaging patients and families in collaborative QI initiatives to improve mental health has become increasingly common, leading to positive impacts on healthcare experiences and outcomes (Francis-Auton et al., 2024; Lachman et al., 2021). However, few descriptions of engagement efforts for an emotional health program targeting youth with chronic health conditions exist. The American Board of Pediatrics Roadmap (ABP) for Emotional Health Project (hereafter referred to as the Roadmap project) is an initiative that includes a QI project aimed at equipping health professionals with the tools and resources necessary to make assessing emotional health standard care for pediatric patients with chronic conditions.
This paper describes the engagement methods used in the Roadmap project, using the Participation Choice Points Model to demonstrate the depth of engagement across the lifespan of the project. This Model delineates five levels of community involvement: inform, consult, involve, collaborate, and empower and describes levels of involvement as well as goals and outcomes. Further, it has been effectively used to describe engagement during the partnering, design, data collection, analysis, dissemination, and action phases of a project (Vaughn & Jacquez, 2020).
To facilitate addressing disparities in emotional health assessment, we anchored our approach in health equity. Parsons et al. (2021) outlined practices for pursuing equity in QI projects, including establishing equity as an essential focus, measuring equity, leading from lived experience, co-production across the research process, redistributing power, practicing a growth mindset, and engaging beyond the healthcare system. To illustrate the application of these practices, we share brief perspectives on the meaningfulness and impact of engagement from an adult patient with a childhood chronic illness, a parent, and a QI team member. The paper concludes with lessons learned that can be applied to future QI initiatives.
Methods
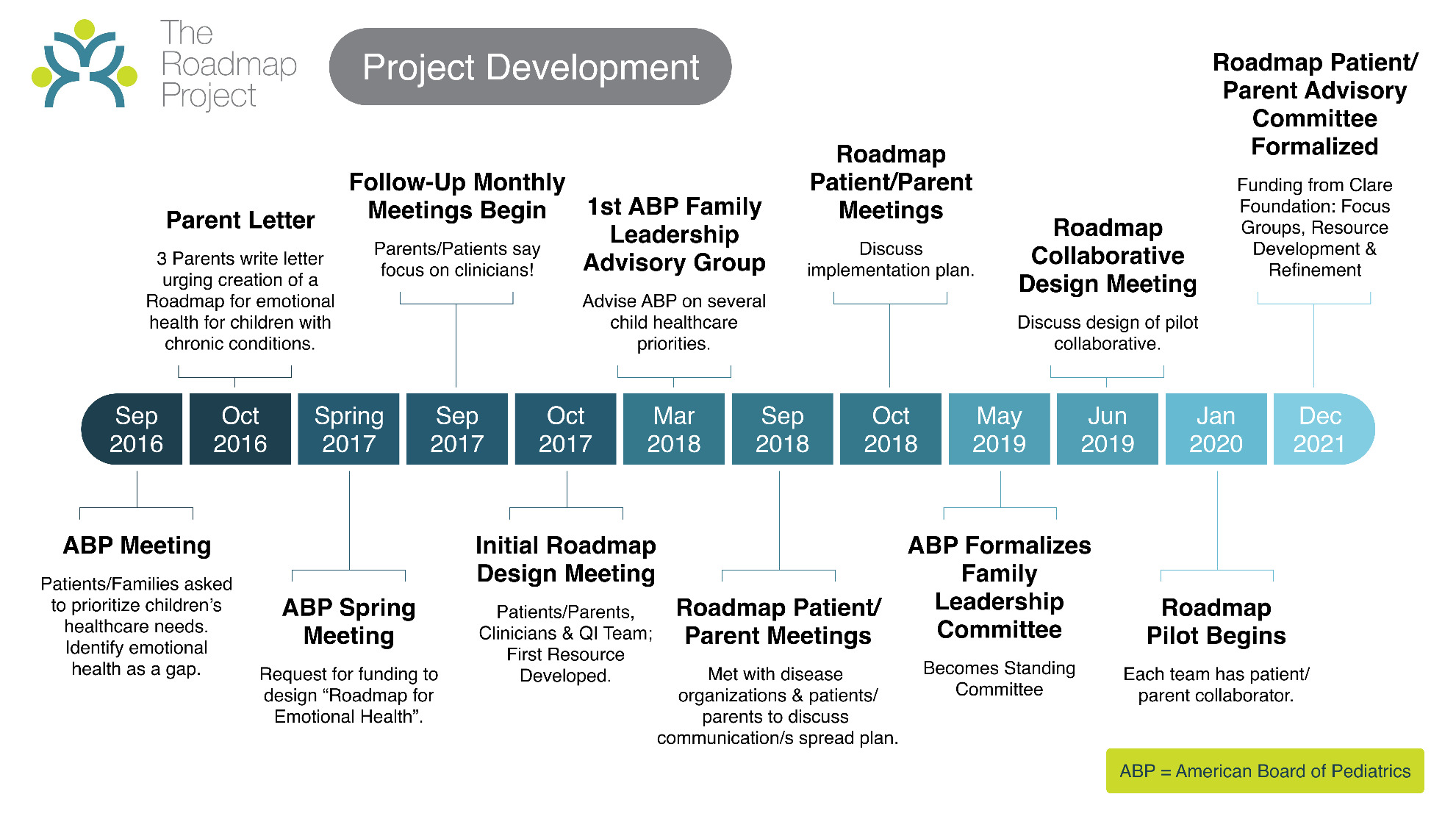
The Roadmap project aimed to maintain patient/family involvement at the collaborate or empower levels, meaning patients/families led some decision-making, particularly in the initial planning phases, and continued to influence decisions during implementation and as the project evolved. In doing so, the process incorporated equity QI practices (see Table 1). Below, we describe the process (see Figure 1 for timeline) and engagement outcomes from the perspectives of collaborators and QI team partners.
Partnership Phase
The idea for the Roadmap project originated from an ABP meeting where over 30 patients and family members shared their priorities for pediatric care (see Pickles et al., 2020 for details, including funding). They reached a consensus that mental health needed to be addressed, especially for children with chronic conditions and their families. Within a year, the ABP funded the “Roadmap for Emotional Health” project (see Lannon et al., 2024 for details of the program), aimed at supporting youth with chronic conditions and their families. Patients and caregivers were invited to co-design the project’s goals, strategies, and measures, while clinicians and other quality improvement professionals contributed their expertise.
Following the inception of the project, a Patient and Parent Advisory Group (PPAG) was assembled. The PPAG met quarterly to biannually as the project progressed. Membership in this group was intentionally fluid to accommodate the varying demands of patients’ and families’ lives. Meetings were offered virtually with multiple time options, and patient/family collaborators received up-front travel support, $250 compensation (prep and virtual meeting), or $25 per hour compensation for their participation. Within this structure, the PPAG led, supported, and completed research activities across the design, data collection, analysis, and dissemination and action stages. Demographics are in Table 2. Example activities are outlined in Table 1.
Design Phase
During the design phase, parents and family members participated in regular meetings. All patient and family collaborators agreed that the intervention should focus on educating and supporting clinicians in assessing emotional health rather than being patient- and family-facing. This direction was adopted. The involvement of patient/family collaborators in the decision-making process redistributed the power of intervention design, typically held by the project team, and shared it with those with lived experience. Consistent with equity principles, the project was led by those with lived experience.
Pilot/Data Collection Phase
The project created a QI toolkit containing strategies and resources to help clinicians address emotional health (Pickles et al., 2020). PPAG and QI project team members collaborated on the development of project resources, including a method for addressing emotional health (Normalize, Ask, Pause & Connect: Sood et al., 2022). The PPAG also provided feedback on the measures for assessing process improvement. Next, a 16-month pilot effort engaged 11 clinical teams from nine children’s hospitals in testing the strategies and metrics.
Clinical teams in both inpatient and outpatient settings, as well as pediatric training programs, tested the toolkit in their practices to improve how they address emotional health. Patients/families collaborated on monthly action period calls. They developed language for teams to use when asking families about their emotional health and proposed potential solutions for teams to test, exemplifying how lived experience was integrated. Training program directors found Roadmap strategies helpful for pediatric trainees and their feedback helped to refine the change package which was used to develop an ABP Maintenance Certification activity (Chawla et al., 2024). The first cohort of pediatricians completing the online MOC activity documented an increase from 21% to 77% in clinical encounters addressing emotional health (Lannon et al., 2024).
One significant outcome of patient/family involvement during the pilot was a workshop focused on addressing disparities in emotional health assessment. The workshop featured a panel of three Black parents and a young Black adult who shared their experiences of being Black, living with a chronic condition, and interacting with the healthcare system. Their insights were summarized into valuable resources for clinicians and trainees including a peer-reviewed publication (Kinebrew et al., 2023). Incorporating these resources into the project demonstrates its commitment to the growth mindset principle. Additionally, by centering equity, these resources help teams better understand how to approach Black families about emotional health concerns.
Dissemination & Action Phases
Patients and families played a significant role in the dissemination and action phases of the Roadmap Project, exemplifying the principle of co-production. Patients and families co-authored several papers (Kinebrew et al., 2023; Pickles et al., 2020; Rosenberg et al., 2024). One of these (Kinebrew et al., 2023) ranked among the top ten most-read articles in the Journal of Hospital Medicine in 2023. This paper in particular highlighted how Roadmap could address racial health disparities. Patients and parents also co-presented at multiple national conferences, at Grand Rounds nationally, and authored online content. In total, more than ten presentations highlighted patient or parent perspectives, and more than nine addressed health disparities within the project’s context. Additionally, PPAG members contributed to blog posts about the project, helping to spread the message that emotional health is crucial for marginalized populations. Several of the Roadmap patient/family collaborators were members of ABP committees. The ABP developed the ABP’s Family Leadership Committee, recognizing the value of sustaining a group of partners with lived experience. This standing group represents the patients’ voice in guiding ABP strategy.
Engagement Perspectives
V. Robyn Kinebrew, MA
As a parent of twins with Sickle Cell Disease, I wondered what I could do to make the journey easier for other families. My engagement in the Roadmap project began with the meeting at the ABP. I have been honored to continue involvement in a project that centers on lived experiences of patients and their families and consults with them every step of the way. I’ve found my thoughts and ideas are valued and the team respects what I have to offer, Projects are more meaningful and effective when they incorporate the diverse voices of individuals who have personal perspectives and direct experience related to the projects intended recipients. Partnering with patients and their families helps ensure equitable and focused outcomes.
Megan Roswick-Didier
As a patient living with congenital heart disease, I have experienced the gap in healthcare between addressing physical health and supporting emotional well-being. While clinicians focused on my physical condition, my mental health was often overlooked, fueling my commitment to ensuring healthcare providers prioritize patients’ emotional well-being. This led to my involvement in the Roadmap project. Through this work, I’ve seen how amplifying the patient’s voice and involving patients as collaborators can transform conversations and outcomes, aligning them with community needs. This approach promotes a more inclusive, equitable healthcare system. Each opportunity to contribute to discussions, co-present or co-author strengthens my ability to share my experiences, bridge communication gaps, and advocate effectively for the patient perspective.
Carole Lannon, MD, MPH
As the project lead for Roadmap, I am committed to ensuring that the patient/family voice remains at the center of our work. Patient and family partners are essential to this work. Their voices are always at the forefront of my mind. As we work to spread Roadmap strategies and resources, patients and families ensure that clinicians understand the “why”. We encourage teams to partner with patients/families. We would not be achieving the results we have if the work had not been focused on what patients/families need.
Conclusions
We utilized community-engaged research and equity models (Parsons et al., 2021; Vaughn & Jacquez, 2020) to describe patient and family engagement in the Roadmap project. Using this model increases the reproducibility of the Roadmap approach for other QI teams and researchers. Other engagement approaches were considered, such as community-based participatory research (CBPR) and human-centered design (HCD), but time and resource constraints prohibited use of these models with fidelity. The key elements that made Roadmap successful from a community engagement perspective were centering the patient voice, striving for equity, and sharing decision-making when possible. Patient perspectives enhanced the project by helping clinicians understand patient and family needs. The high level of partnership throughout the project ensured the intervention’s acceptability, made it actionable (e.g., providing tangible resources applicable to families), increased equity (as defined by Parsons et al., 2021), and provided patients/parents with opportunities to make non-traditional contributions such as co-authoring scientific presentations and publications.
Limitations
The Roadmap project engagement model is not without limitations. First, participants were self-selected and may not be representative of all families seeking care in subspecialty clinics. Second, parents/patients had limited opportunities to share power or lead decision-making due to the nature of the project (i.e. need to align with ABP goals). Third, although we utilized two models to describe the engagement process, this may have failed to capture the true complexity of the engagement, and insufficiently describe challenges related to sustaining engagement over time.
Lessons Learned
The engagement of patients and families in the Project has yielded several valuable lessons. First, commensurate with other co-produced health products, incorporating lived experience into design increases intervention effectiveness and outcomes (David et al., 2018). Second, co-production can lead to more innovative solutions (Seid et al., 2021), as patients and families often provide unique insights that professionals might overlook, such as how to address health disparities (e.g., the Impact of being Black article and resources). Third, although logistical barriers (e.g., attendance, compensation) persist, overcoming them is worthwhile as patients/families reflect that participation has fostered a sense of ownership and empowerment. Fourth, sustaining engagement requires intentionality and resources. Last, this collaboration has underscored the need for continuous communication and feedback loops to adapt and refine strategies based on real-world experiences.
Based on our experience with engagement in the Roadmap Project, we recommend that QI projects utilize community-engaged research models to organize and describe patient/family involvement. Furthermore, integrating equity principles helps to ensure that specific needs and challenges that might otherwise be overlooked are addressed, contributes to more holistic and equitable healthcare solutions.