INTRODUCTION
Jamaica (JA) is a low-to-middle income Caribbean country that is experiencing increasing rates of noncommunicable diseases (NCDs) (e.g., diabetes, heart disease, stroke – see Bourne, 2009; Ferguson et al., 2010, 2011; Kramer et al., 2018; Moran et al., 2014; Yisahak et al., 2014). For example, a national JA survey reported prevalence of diabetes increased from 7.2 to 7.9% and hypertension increased from 21 to 25% between 2000-2001 to 2007-2008 (Ferguson et al., 2011). Additionally, complications related to NCDs and social determinants (e.g., limited access to care; neighborhood functioning) persist (Cunningham-Myrie et al., 2013, 2015, 2018; East et al., 2015; Harris et al., 2014; Mitchell-Fearon et al., 2014).
Limited engagement in physical activity is a key factor that is contributing to growing rates of NCDs in JA (Cunningham-Myrie et al., 2013; Ministry of Health and Wellness, n.d.). The JA Ministry of Health and Wellness (n.d.) is conducting a national physical activity campaign called “Jamaica Moves”. However, residents in remote, rural areas have less access to exercise facilities and safe roads, and may be less likely to engage in physical activity and other health lifestyle behaviors (Cunningham-Myrie et al., 2015). Also, although JA has a free healthcare system, including prescription medications, and provides services at more than 20 public hospitals, clinics, and health centers, the system is sorely under-resourced and long wait times persist, especially for rural residents who have great difficulties accessing public facilities (Casey, 2009; Ferguson et al., 2011). This is concerning because residents of rural JA areas are more likely to be diagnosed with NCDs, such as diabetes, than those in urban areas (Cunningham-Myrie et al., 2013).
A national study, which included JA’s 14 parishes, found that women were more likely to be at risk for NCDs than men (Cunningham-Myrie et al., 2018). The study also found that JAs who live in communities with access to recreational spaces are more likely to engage in physical activity (Cunningham-Myrie et al., 2018) and to have reduced risk for NCDs than those who do not have such access. Although studies have shown that JAs understand the importance of lifestyle changes to reduce NCD risks (Wilson et al., 2018), support to engage in these changes are limited for those living in rural and underserved areas. Highly feasible, acceptable community approaches are critically needed to improve reach of health promotion interventions to reduce NCD risk with underserved JAs, particularly those who live in underserved, low-resource, rural JA areas.
A key asset in many rural JA areas are faith-based institutions, with Christianity being the primary religion in the country (Tsang, 2015). Studies have found that Afro-Caribbean persons believe religion is highly important and have high rates of church attendance (Taylor et al., 2010). Also, a few studies have indicated that increased church attendance is associated with improved daily functioning and happiness among JAs (e.g., Bourne, 2009). Yet, few reports exist on how JA churches, which are prevalent in rural JA areas, can be engaged in designing and implementing appropriate religiously-tailored health promotion interventions for improved acceptability, reach, and impact with their church members and the community members they serve.
Community-based participatory research (CBPR) has been used in the U.S. as an approach to address health inequities by engaging faith community members in addressing the health of underserved congregants and community members (Israel et al., 2005, 2013). CBPR-driven health promotion interventions have addressed many health concerns in faith-based settings, such as HIV/STDs (Berkley-Patton et al., 2016, 2018; Derose et al., 2016), fruit/vegetable intake (Campbell et al., 2007), colorectal cancer (Lumpkins et al., 2013), and blood pressure (Whitt-Glover et al., 2017). In these and other studies, faith members have assisted with determining study procedures, recruiting and retaining participants, interpretation of results, and dissemination of research findings. Faith leaders and church members have also contributed to the religiously and culturally tailored design of faith-based interventions to ensure intervention components are appropriate for the church context, acceptable to members, and feasible to implement (Berkley-Patton et al., 2013, 2016, 2018; Derose et al., 2016; Sattin et al., 2016). For example, church-based intervention studies conducted by Berkley-Patton and colleagues (2013, 2016, 2018) focused on HIV education and testing fully engaged African American faith leaders in a CBPR process to design, implement, evaluate, and disseminate the religiously-culturally tailored intervention (Taking It to the Pews [TIPS]). Feasibility and outcome studies indicated that TIPS yielded much higher HIV testing rates (42% versus 59%) than a non-tailored control condition, respectively (Berkley-Patton et al., 2016, 2019). Inclusion of faith leaders/church members in the research process has also been intended to increase ownership and maintenance of the intervention, while increasing the capacity of churches to address existing and emerging health concerns of importance to church and community members. However, limited information is available on how churches have participated in initially establishing the research agenda in partnership with researchers to identify health issues of importance to church and community members in order to make decisions on the design and primary outcomes of planned interventions.
A participatory process that has been used extensively to understand community concerns and guide the determination of the research focus, intervention procedures, and needed cultural tailoring is the use of a community needs assessment process (Sharma et al., 2002). Community needs assessments go beyond simply collecting survey data on community members’ input on health concerns. Instead, needs assessments are conducted as a process that engages community members in determining concerns for which information is sought, approaches to gather this information (e.g., surveys, interviews, community town halls), and discussions on findings with the broader community and smaller constituent groups (e.g., community advisory boards) (Berkley-Patton et al., 2018; Bias et al., 2017; Fawcett et al., 1988; Sharma et al., 2002). A needs assessment focused on health also includes using the information gathered to spur creation of new programs (e.g., health promotion interventions), policies, and practices that, taken together, could positively shift health outcomes and reduce health inequities (CDC, 2013). Although more reports on needs assessments in faith communities are emerging (e.g., Berkley-Patton et al., 2018; Whitt-Glover et al., 2017), to our knowledge, no reports exist on CBPR and needs assessment approaches used to engage JA faith leaders in faith community-based research to improve the health of their church and community members.
Here, we report on our CBPR process used to engage JA faith leaders in conducting a health needs assessment (HNA) process and how HNA findings were used to guide the design of a health promotion intervention in churches from two JA parishes (Saint Ann and Saint Mary). The resulting multilevel, healthy lifestyle intervention, Faith Influencing Transformation (FIT)-JA, aimed to increase diabetes and heart disease awareness and promote physical activity. This report describes the HNA process used to inform the design the multilevel FIT-JA intervention and its religiously-tailored materials/activities packaged in a FIT-JA Tool Kit.
CONTEXTUAL BACKGROUND: THE JAHLMA COMMUNITY ACTION BOARD (CAB)
Using a CBPR approach, a faith-academic partnership (the Jamaican Health Lifestyle Ministry Association; JAHLMA) was developed with church leaders from rural areas in Saint Ann and Saint Mary parishes. The development of the relationship between the JA faith leaders and researchers was led by a senior U.S. pastor (fifth author) who immigrated from JA to the U.S. in the early 1960s and returned regularly to build churches and address health issues in underserved rural areas near his childhood home community in Saint Mary. In seeing the declining health in this area, he approached the first author to meet with the JA faith leaders and share information about the faith-based health promotion research being conducted by the university-based research group that the first author led. This led to meetings with the faith leaders to determine the appropriate approach JA faith leaders could take to address health concerns of their church-community members. In these early meetings, information was also shared on the faith-based health promotion studies conducted in the U.S., including an ongoing diabetes/CVD risk reduction intervention (Project FIT) that had been developed/implemented by African American faith leaders (Berkley-Patton et al., 2018, 2020).
After a little over two years of relationship building with church leaders, the JAHLMA CAB (twenty members from six churches) was formalized. The CAB had ongoing discussions about their churches, congregants, current health-focused projects, the functioning of their churches (e.g., key leaders, flow of church services, how decisions were made, important annual events), church culture, and the health of their congregants and community members. The researchers met in-person with the JAHLMA CAB about three times per year. CAB meetings were held during lunch hour with a full, hot, traditional JA meal served as an incentive to attend the meetings. Additionally, due to the high transportation costs and limited transportation options in JA (e.g., taxi, hitch ride, bus, walk), all CAB members received $20 US to cover their transportation to attend CAB meetings, which increased CAB meeting attendance.
The JAHLMA HEALTH NEEDS ASSESSMENT PROCESS
The JAHLMA CAB’s initial focus was to conduct a HNA process with church-community members to understand health conditions, priority health concerns, and intervention strategies that could be feasibly implemented in limited resource rural church-community settings to address concerns. CAB members were fully engaged in all phases of the HNA process, which included: a) discussing their community’s health concerns and identifying potential relevant home-grown intervention and empirically-tested strategies to include in the HNA survey; b) refining study procedures to appropriately administer the survey in JA Saint Ann and Saint Mary parish churches; c) holding church-community forums to share and gain input on HNA survey findings with a broader group of church-community members; and d) using the HNA survey findings and community forum discussions to ultimately guide the design of a health promotion intervention, as shown in Figure 1 below.
Discussing Health Concerns and Identifying Relevant Potential Intervention Strategies
A national assessment of health and lifestyle behaviors, conducted about every 10 years in JA, reported that, except for hypertension, rates of CVD risks are similar between JA rural and urban dwellers (Ferguson et al., 2011). Still, very little information exists on the health status and health-related behaviors of JAs in rural areas. The JAHLMA CAB discussed the national data and their personal perspectives on the health status and concerns of their church and community members in two CAB meetings. The CABs’ experiential knowledge of health conditions they witnessed most frequently in their communities aligned fairly well with the national data on leading causes of death (e.g., diabetes, CVD). They commented that most of their parishioners did not have private health insurance or a medical home, and therefore most used local free clinics as their primary health home. They were in agreement that access to healthcare services, including health screenings, annual visits, and medications, was limited for their church-community members due to the long distance, cost of travel, and time from work to see health providers at the nearest clinic. They also discussed health issues that were difficult to address in clinics, such as vision problems, allergies, and limited availability of medications in free clinics. HIV/AIDS was also discussed along with related stigmatizing beliefs, however, the CAB did not think it was as large of a problem as some of the other health conditions.
Based on their knowledge and experiences, they identified the leading health concerns among their church-community members as diabetes, heart disease, and asthma. They believed health conditions, such as cancer and other diseases, were of less concern. These discussions resulted in five health categories of concern that would be the focus of the HNA survey: asthma, diabetes, CVD/stroke, hunger, and access to healthcare and related services. The CAB also wanted to include an area of focus for potential strategies that could cut across the five areas of concern and be delivered in church services. Therefore, a sixth category on church-based strategies was also included on the survey. The research team used the information gathered from these discussions to draft a sample HNA.
The next CAB meeting was used to review the draft survey, which included demographic and other health-related items (e.g., health screenings, health conditions diagnosed), and listed potential health promotion strategies that would be rated of importance and feasibility to address each of the concern areas. To efficiently guide this process, the research team had the CAB use planning tools, which included planning pages that indicated the potential strategies for the intervention, the church level outlet for dissemination of the strategy, and existing community resources that could help support implementation and maintenance of the strategy. CAB members edited and added the list of strategies, which yielded a total of 75 potential strategies. For example, among the 16 potential diabetes health promotion strategies, exemplar items included: “Provide diabetes education” and “Provide seminars on proper exercises that can be done at home.”
Refining Study Procedures and Administering HNA surveys in JA Churches
The CAB meetings were then used to refine and finalize the survey, which was ultimately nine pages (three pages on demographics and health-related questions and one page for each of the six health concerns areas). CAB members further deleted, combined, and edited the potential strategies under each category, which resulted in 61 strategies that were included on the survey. The CAB also made edits to other survey questions to improve the comprehension of the questions for their members. They also determined the most appropriate procedures to administer the HNA survey with church and community members, which included reading the survey aloud to participants in the church sanctuary.
In discussing appropriate procedures to administer the survey, the faith leaders wanted the surveys to be completed by members immediately after Sunday church services in order to get the best participation. They also felt it best to have the members of the four smaller churches represented on the CAB to come to services at the two larger churches, led by senior influential leaders, for joint fellowship and survey completion. Leading up to the HNA survey events, JAHLMA CAB leaders informed their members about the need to increase their focus on health promotion, the importance of their engagement in research to understand the health needs of their church-community members, and place/time of the upcoming survey event. On the Sunday on which the surveys were held, the lead pastors in the two hosting churches spoke about the importance of health, introduced the research team during the service, and encouraged their members to stay after the services to learn more about the study. These pastoral efforts contributed to 242 adult church and community members (out of about 270 adults in attendance at survey events) completing the HNA. The research team read the entire survey aloud and allowed time for participants to answer the questions. Team members were also available to help participants individually as needed.
Holding Church Community Forums to Feedback HNA Survey Findings
Once the research team completed the HNA survey data analysis (frequencies and means were used to convey the findings), the team met with the JAHLMA CAB to discuss the findings and plan how to disseminate the findings with the broader church community, especially with churches that participated in the survey. CAB members also discussed potential concerns that weren’t addressed in the survey, including poor access to medications, such as blood pressure and diabetes medications, and the low health literacy of their members. They also expressed the need to initially focus on intervention strategies that were feasible and in their control, considering the limited opportunities to partner with health agencies on an ongoing basis due to the rurality of their locations from larger municipalities where most health services were delivered. Additionally, the CAB felt it was best to hold community forums at the two larger participating churches where the survey was held to feedback the HNA findings. They invited the pastors and members of the four smaller churches that participated in the HNA to participate in the forums at either of these churches.
About 90 church-community members from the six churches attended forums at the two larger rural churches to discuss HNA-identified concerns (e.g., diabetes/CVD, limited fruit/vegetable intake, health care access). The forums lasted one hour, and common themes were identified based on topics that commanded the most time at both forums. Common thematic concerns voiced by forum and CAB attendees included the need for: more fresh fruits/vegetables, gardening training and supplies, healthy food sharing programs, access to exercise programs/equipment, and diabetes/CVD education. Other themes included high cost of private health insurance and medications, and overcrowded free clinics. Attendees commented on the need to develop diabetes/CVD prevention and healthy eating/exercise programs in church settings and to tap church social support and free WhatsApp messaging to promote preventive behaviors. This feedback from church-community members was taken into consideration by the JAHLMA CAB in designing the health promotion intervention’s research focus and its components.
Designing the Project FIT-JA Intervention
The CAB determined that the health promotion intervention should focus on diabetes and heart disease since these health conditions had overlapping risk factors and were highly prioritized on the survey and in community forum discussions. In doing so, the CAB inquired more about the diabetes/CVD studies conducted by the research team with African American churches in the U.S. The CAB was strongly encouraged to wholly design their health promotion intervention based on HNA findings and community forum discussions from scratch. However, they were quite determined to use the existing Project FIT intervention model as the starting point for designing their intervention. From their perspective, they felt complete ownership of their design process in adapting FIT-JA from the U.S.-based Project FIT. Therefore, more information was provided on the Project FIT study, which focused on diabetes/CVD risk reduction using a religiously-tailored materials/activities packaged in a Project FIT Tool Kit. In making the decision to focus on diabetes and the Project FIT model, the CAB identified Project FIT Tool Kit materials/activities that they believed would be most appropriate to promote healthy behaviors and could fit naturally into their regular church services for increase reach and impact.
Intervention Focus, Name, and Logo: JAHLMA Consideration of JA Culture
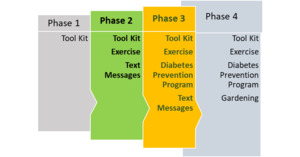
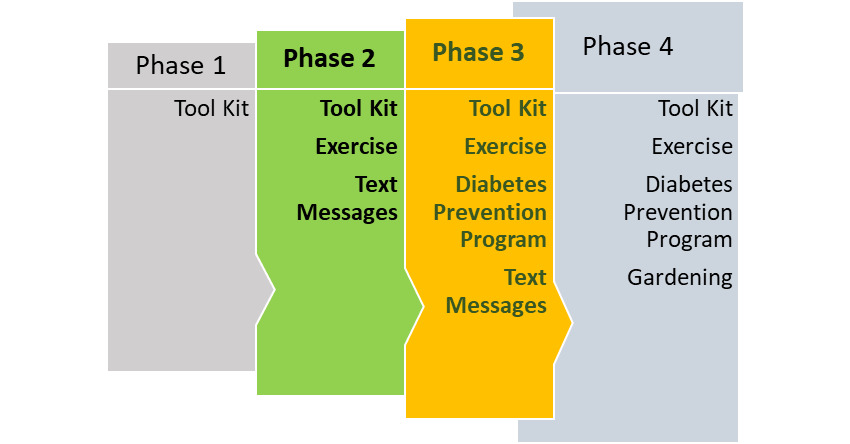
The JAHLMA CAB expressed great interest in adapting the Kansas City Project FIT intervention to the JA church context. Interestingly, they commented that with the advent of social media, JAs increasingly wanted to adopt the American culture. Despite their concerns that this change in culture contributed to JA’s limited engagement in healthy lifestyle behaviors and poor health conditions among JAs, they believed that a health promotion intervention that was adapted from a successful American model would be appealing to their members. Therefore, they decided to maintain the name of the project, but include JA in the name, resulting in Project FIT-JA, with the logo including this change. They also decided to change the color of the original logo and toolkit materials from blue/gold to colors that represented JA: green/yellow/black. However, unlike the original intervention which included the CDC’s evidence-based 22-session Diabetes Prevention Program adapted for the African American church context in a weekly group-level format (see Berkley-Patton et al., 2020 for a description), the CAB decided instead to implement weekly group exercise as a key behavioral diabetes risk reduction component to provide to their church-community members. This potential strategy was strongly endorsed as important in community forums meeting. The CAB determined that due to limited resources, the development of religiously-tailored tools (e.g., sermon guides, church bulletins) quickly followed by development of WhatsApp text messages to promote physical activity along with church-based group exercise would be feasible to quickly implement as the first two phases of FIT-JA. They also decided that future FIT-JA component phases would be more time and cost intensive, but would incorporate the Diabetes Prevention Program and gardening, as shown in Figure 2.
Next, the CAB began to tailor the multilevel Project FIT components, as needed, to their JA church context while maintaining the core intervention components that aligned with priority health strategies identified. They made decisions on which original Project FIT materials/activities would be adapted for packaging in a FIT-JA Tool Kit. The selected tool components included: self-help materials (e.g., commitment pledge, risk checklist, bible bookmarks, other printed materials; individual/interpersonal levels), exercise classes (group level), sermons and responsive readings (church level), and WhatsApp text messages (church-community level) to promote healthy lifestyle behaviors. Because limited access to healthcare services was a tremendous concern among their members, they also wanted to include a resource list of health services on the back of many of the tools, which included information on the location, types of services, and hours of operation for the health services. Biblical scriptures were included on all original materials to tap the spiritual aspects of members’ behavior change and religious beliefs and were deemed highly appropriate to be maintained for the FIT-JA materials. The CAB also identified strategies for delivery of each FIT-JA material/activity through multilevel church outlets by a team of trained church leaders. Additionally, instead of calling the trained church leaders “church health liaisons,” as was done in Project FIT, they named the FIT-JA trained church leaders “ambassadors” to suggest that their role would be to deliver hope and goodwill for improved church-community health through church multilevel outlets, as described below.
Individual-Level
Self-help materials. The CAB reviewed the original Project FIT commitment pledge which was designed for members to pledge that they would engage in specific healthy behaviors, including eating more fruits and vegetables, exercising 150 minutes a week, reducing intake of salty and fatty foods, and supporting each other in their efforts to engage in these activities. Additionally, the CAB expressed interest in the commitment cards being distributed by ushers during Sunday morning services as members entered the sanctuary and possibly having members read the commitment cards aloud together. The members would then be asked to sign the cards and retain them in a location where they could see it daily, like their Bible. They also believed the commitment cards would need to be distributed again when members enrolled as participants in the intervention study. A risk checklist included the primary risks (e.g., age?; gender?; high blood pressure?) for diabetes/CVD and encouraged members to support each other in addressing these risks. They also selected Bible bookmarks to be included in the FIT-JA Tool Kit, because they believed this was a good strategy to have a visual reminder to engage in healthy behaviors that members would see daily as they read their Bibles. Lastly, several brochures from the American Diabetes Association and the American Heart Association were included in the self-help materials. The JAHLMA CAB felt that these were credible sources of health information that were highly recognized/respected by their church-community members.
Group Level
Physical activity. Exercise was selected as the key behavioral diabetes risk reduction component that was needed and was feasible to address at the group-level, especially with limited resources. The CAB believed that their church members would be motivated to attend a weekly group exercise program if: pastors promoted the exercise program from the pulpit; their children could attend; and if it could be a fun event. They also stated that group exercise could be a way for members to support each other and could also be seen as a social event that could also be attended by community members. To ensure the exercise program would take place each week, regardless of resources, they determined that at least one to two ambassadors from each church should lead low-impact exercise, such as walking and dancing. For example, low-impact movement would be done to well-known church songs like “Father Abraham”. They also planned for group exercise participants to be weighed each week. They planned to open/close each exercise session with prayers, reading of scriptures, and sharing reflections on personal experiences of participants as it related to exercise and other healthy behaviors.
Church-Level
Sermon guides. Similar to the original Project FIT, the faith leaders believed that the influence of the pastor was a critical component needed to motivate church-community members to engage in healthy behaviors, including exercise. They reviewed existing sermon guides from Project FIT. The faith leaders believed that while a guide would be helpful to provide exemplar content for a sermon and accurate information to promote, they also believed that no one could quite tell pastors how to preach, therefore, emphasizing that this tool was to be used as a guide to assist pastors in incorporating healthy messages in their sermons.
Responsive reading. A responsive reading was adapted from the original Project FIT study. This tool was designed as a “call and response” reading with the pastor serving as the “Leader” and the congregants serving as “People” responders, as shown in Figure 3. The intent of this tool was to share data about the impact of diabetes/CVD among JAs and to unify congregations in committing to healthy behaviors by verbalizing their commitment. The responsive reading was intended to be read during Sunday morning church services when most members would be participating in the worship services. To finalize the responsive reading, the CAB members read the final draft out loud with a senior pastor serving the role as the leader to test the flow and verve of this tool.
Church-Community-Level
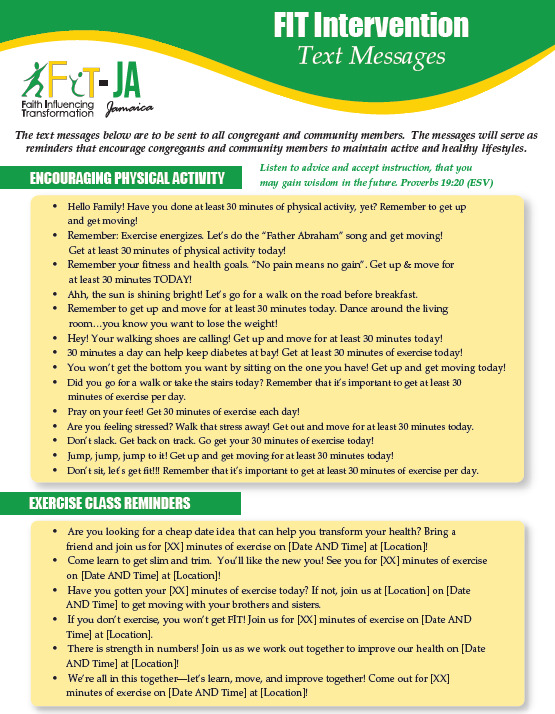
WhatsApp text messages. The HNA findings indicated that 53% of participants reported they had a smartphone and 61% used WhatsApp on a regular basis. Additionally, the CAB faith leaders had shared that they were already using WhatsApp to communicate with church members. Therefore, the WhatsApp text tool was selected by CAB members as a strategy to provide ongoing motivational messages to encourage healthy lifestyles and as a reminder to attend the group exercise sessions. To create this tool, CAB members read through original Project FIT text message tool. Then, they made decisions on whether to keep or edit the text messages. Although many remained unchanged, small edits were made to several of the messages to better reflect terms used by JAs and the JA context. For example, the message “Tonight’s the night! Go for a walk around the block after dinner tonight,” was edited to read as "Ahh, the sun is shining bright! Let’s go for a walk on the road before breakfast," to reflect the sunny JA climate and note that most walking in rural JA areas is done in the road, since sidewalks are extremely limited in these areas. They designated that text messages would be sent two to three times per week to church-community members.
DISCUSSION
To our knowledge, this is the first report on the development of a health promotion intervention that fully engaged the faith community in the intervention design/research process in JA. Akin to key CBPR principles, the focus of the intervention, diabetes/CVD risk reduction, emerged from concerns identified by the faith community (Israel et al., 2005, 2013). Also, faith leaders were engaged in nearly every phase of the research process, as recommended when using CBPR approaches (e.g., Duran, 2017). By collaborating with the highly active CAB and listening to rural communities via a HNA process inclusive of a survey and community forums, the community’s voices directly guided the design of the resulting multilevel FIT-JA intervention tailored for rural JA faith communities. There were several lessons learned throughout the CAB development, HNA process, and intervention design process that could be beneficial to others who seek to collaborate on development and eventually implementation with faith leaders in low-resource areas.
First, although relationship building with collaborating partners may take time to build trust and mutual understanding, this time investment can pay off generously in being able to more efficiently accomplish research goals (e.g., Duran, 2017). Because research resources were limited and travel to JA only occurred only two to three times per year, each trip had to be optimized in getting things done. The use of planning tools, having clear next steps, and returning to the next meeting with demonstrated productivity in following through on next steps, greatly contributed to quickly advancing the research process and in building trust from knowing that CAB and community voices had been heard and acted on. We have found that these strategies have also greatly contributed to increased efficiencies in conducting research with our faith-based KC FAITH Initiative CAB, which meets quarterly with about 30 representatives from faith, health, community, and academic organizations (Berkley-Patton et al., 2018). First, early discussions with the JAHLMA CAB about community health concerns yielded priority health issues that aligned with those heard from community members in community forums and were reflected in the HNA findings. This knowledge base highlights the CBPR principle that community members’ knowledge about their local community is important to co-learning and understanding community needs (CDC, 2013; Sharma et al., 2002). In this project, the experiential knowledge of the faith leaders about the health of the communities they serve may be even more relevant and timely than national, and possibly local, reports, especially considering they regularly visit the sick and shut-in and share prayers with caregivers of sick loved ones – some who may not be able to access health services. Additionally, their experiential knowledge may be reflective of their personal health. During CAB meetings, the faith leaders often talked about their personal health struggles and lifestyle changes they had made to improve their health. A recent study with JA faith leaders indicated that they were experiencing high rates of diabetes, hypertension, and cholesterol and were at great risk of life-threatening NCDs (Bourne, 2020). Future work is needed to understand how JA faith leaders can be further engaged in the development of church-community-based health promotion interventions due to their personal health status and the health of the communities they serve.
Second, being sensitive to CAB members’ basic needs that could limit their attendance in CAB meetings and increase their active participation in the meeting was critical. We quickly learned that transportation costs from rural areas were particularly high and a huge barrier that limited attendance. The CAB wanted to meet in Ocho Rios, which they considered to be a central location, but which was still a considerable distance for faith leaders from some of the most rural areas in the St. Mary and St. Ann parishes. Therefore, CAB members were provided with $20 U.S. to cover transportation costs to attend meetings and with a traditional JA hot lunch (e.g., brown stew chicken, fish, rice and peas, cabbage), as advised by the CAB. We also learned that using WhatsApp as the primary source of communication was critical to staying in touch with the rural faith leaders in-between meetings. Most had cellphones and were able to access WhatsApp even in the most rural areas, which was consistent with our HNA findings and other studies (e.g., Dunn & Dunn, 2007). However, most did not have access to a computer or regular access to the internet, thereby making it difficult to share materials from abroad and to get timely responses on sent documents. Despite the growing reports in the CBPR literature on the importance of understanding the health concerns and needs of underserved faith communities (e.g., Berkley-Patton et al., 2018; Whitt-Glover et al., 2017), less information is available on understanding and responding to the needs of faith leaders who are fully engaged in serving their community and working collaboratively with researchers. More information on this practice can help provide information on strategies to create highly functioning, faith-based CABs and could possibly lead to increased timeliness and efficiencies in responding to community-identified needs.
Third, interestingly, the faith leaders insisted on adapting one of the existing health promotion interventions, Project FIT, to the JA context because of the potential appeal of implementing an American project. However, except for the colors, some minor changes to terms used, and inclusion of JA data on diabetes and lifestyle behaviors, they maintained the majority of the content of the original multilevel Project FIT tools. They believed that most of the materials and activities were relevant and would be widely acceptable to their community members “as-is” and could be delivered through similar multilevel outlets (e.g., individual, group exercise, church services, and WhatsApp text messages to church-community levels) with their church-community members. This was surprising, especially considering JA has such a rich, distinctive cultural history (Murrell, 2010). Still, they were concerned that implementing the Diabetes Prevention Program would be a larger commitment and believed that implementing group exercise would be more manageable – and that the DPP could be added later as their capacity to engage in research increased. This is a good example of the CAB balancing their responsiveness to community needs with understanding their capacity to deliver specific intervention components.
Lastly, the CBPR approach used led to a true ownership of the intervention by the CAB members. The CAB selected/tailored intervention components that they felt best to implement in churches and would be widely accepted by their community, a key outcome of using a CBPR approach (Arroyo-Johnson et al., 2015). This process provided faith leaders with opportunities to step into expanded leadership roles and increase the capacity within their limited-resource, rural areas to address the health concerns of their church-community members. Capacity building to address existing and newly emerging community concerns is an important outcome of using a CBPR approach and demonstrates the ability for the community to further impact problems that burden their communities (Kaholokula, 2013). Ultimately, the hope is that the CBPR process used will have benefits beyond the current project and will extend to the development and implementation of other health promotion interventions based on community input and actions.
ACKNOWLEDGEMENTS
We would like to thank the JAHLMA CAB members on their commitment to collaborate in research to improve the health of their church and community members.
FUNDING SOURCE
This work was funded by the University of Missouri-Kansas City School of Medicine.